Loading... Please wait...
Loading... Please wait...
Already have an account?
Login to check loyalty balance or redeem rewards
- Home
- Blog
BLOG
Chikungunya Virus
Posted on 1st Oct 2014 @ 12:17 PM
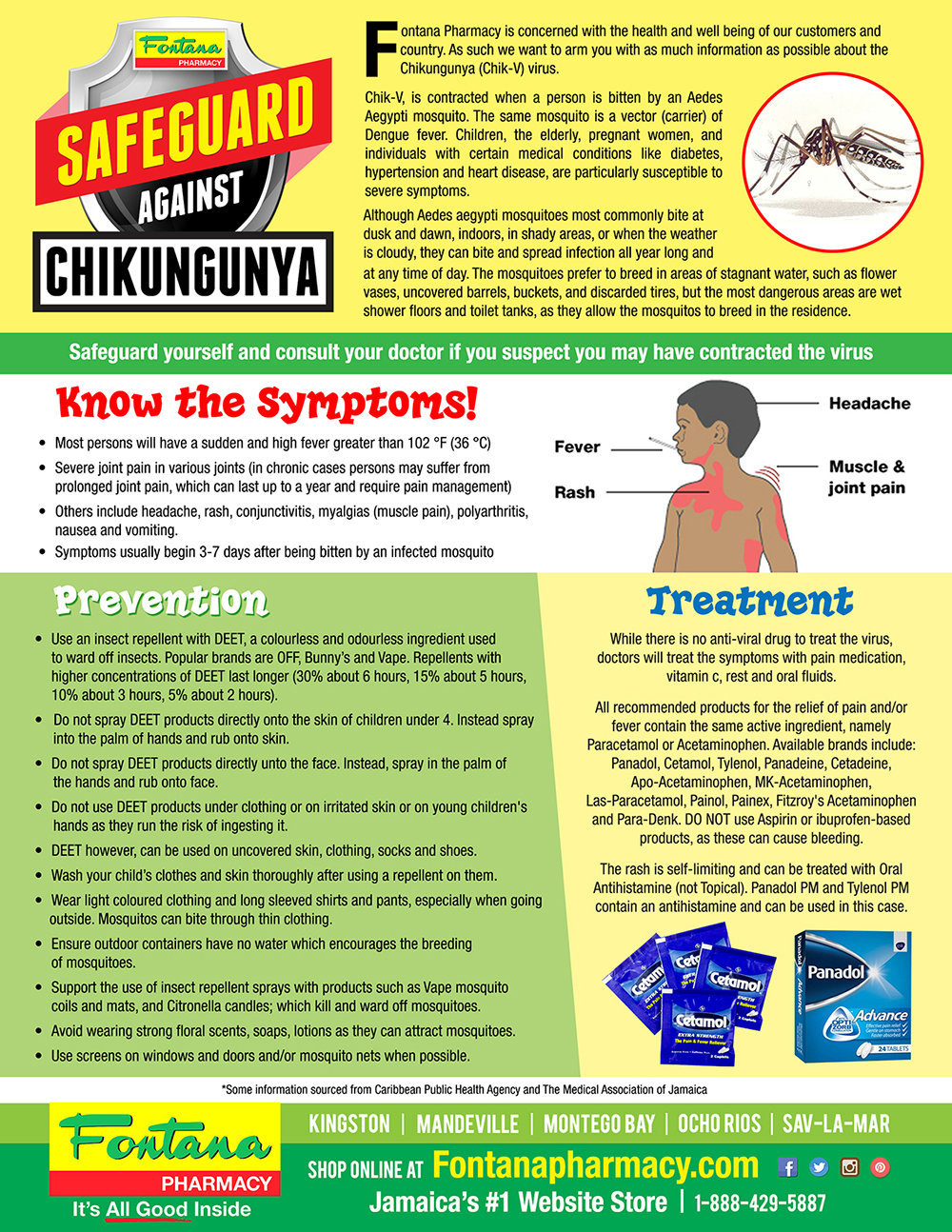
Safeguard yourself and consult your doctor if you suspect you may have contracted the virus.
Chikungunya is caused by the chikungunya virus (CHIKV), an arthropod-borne virus (arbovirus). Chikungunya is a member of the Alphavirus genus in the family Togaviridae. There are 29 different types of alphaviruses that cause diseases in humans and other mammals. These species of arboviruses have been classified into 7 antigenic complexes: Barmah Forest (BF), Eastern equine encephalitis (EEE), Middelburg (MID), Ndumu (NDU), Semliki Forest (SF), Venezuelan equine encephalitis (VEE), and Western equine encephalitis (WEE).
Alphaviruses can be divided into New World and Old World viruses. These two groups have evolved distinct ways of interacting with their respective hosts and differ in for instance their pathogenicity, and tropism. Chikungunya virus is part of the Semliki Forest SF group of Old World Alphaviruses. Predominantly New World viruses are associated with encephalitis, whereas poly-arthritis and a rash is predominantly associated with Old World alphaviruses. Although chikungunya virus is a member of the arthritogenic alphaviruses, there are also cases of meningoencephalitis and haemorrhagic disease.
The Alphavirus genus includes besides Chikungunya virus also O'nyong'nyong virus (ONNV) and Ross River virus (RRV). Chikungunya and O’nyong nyong virus have 85% similarities in their genome. The O'nyong'nyong virus causes disease with symptoms very similar to chikungunya virus. It is also transmitted by mosquito's and the disease symptoms include arthritis, fever and rashes. This virus is so far limited to African countries mainly Uganda. It is not known to be fatal. The Ross River virus causes rashes and arthritis. This virus is epidemic in Australia and some of the surrounding islands. This virus is also transmitted by mosquitoes.
Chikungunya virus is a small (about 60–70 nm-diameter), spherical, enveloped, positive-strand RNA virus (see figure 1). Early 2006, the complete sequence of a chikungunya isolate from Reunion Island was made available through NCBI/ GenBank accession no. DQ443544.1. The virion consists of an envelope and a nucleocapsid. The chikungunya virus genome is 11,805 nucleotides long and encodes for two polyproteins – the non-structural polyprotein consisting of four proteins (nsP1, nsP2, nsP3 and nsP4) and the structural polyprotein consisting of five proteins (Capsid, E3, E2, 6K and E1) (see figure 2). The 5’ end of the RNA molecule is capped with a 7-methylguanosine while the 3’ end is poly-adenylated. A subgenomic positive-strand RNA referred to as 26SRNA is transcribed from a negative-stranded RNA intermediate. This RNA serves as the mRNA for the synthesis of the viral structural proteins. Alphaviruses have conserved domains that play an important role in the regulation of viral RNA synthesis. These domains are found at the 5’ and 3’ ends as well as at the intergenic region. The E1 and E2 glycoproteins are expected to form heterodimers that associate as trimeric spikes on the viral surface covering the surface evenly. The envelope glycoproteins play a role in attachment to cells.
Virions located on the surface of the cell membrane enter the host cells by fusion and endocytosis of the viral envelope. The uncoating of the virions occurs in the cytoplasm. The site of mRNA transcription is in the cell cytoplasm. Replication is not restricted to a particular tissue or organ of the host so the virus replication occurs in various organs. The insect host initiates the virus replication. The genome replication is done in the cytoplasm (see figure 3).
Please see. http://www.chikungunyavirusnet.com/chikungunya-virus.html
Chikungunya Signs & Clinical Symptoms
The incubation period of chikungunya disease is from 2-6 days with symptoms usually appearing 4–7 d post-infection. If you have become infected with the chikungunya virus, you will noticed several symptoms some of which might include:
- Rash
- Pain in the Lower Back
- Joint Pain (with or without the presence of swelling)
- Vomiting
- Nausea
- Headaches
- Chills
- Fevers
Upon infection, chikungunya tends to present itself in two phases, the acute phase and the chronic phase:
Acute phase
The acute phase of chikungunya infection typically lasts from a few days to a couple of weeks. Characteristics of the acute phase include an abrupt onset of chills, fever reaching up to 40 °C (104 °F), vomiting, nausea, head ache, arthralgia (joint pain), and in some cases, maculopapular rash characterized by raised, spotted lesions. Severe joint and muscular pain is the main and the most problematic symptom of chikungunya. The pain is so intense that makes movement very difficult and prostrates its victims.
Typically, the fever lasts for two days and then ends abruptly. However, other symptoms like joint pain, intense headache, insomnia and an extreme degree of prostration, can last for about 5 to 7 days. During the acute phase, the viral load can reach 10E8 viral particles per ml of blood. The virus has been shown to infect epithelial and endothelial cells, primary fibroblasts and monocyte-derived macrophages, explaining the involvement of muscles, joints, and skin connective tissues.
Chronic phase
The chronic stage of chikungunya is characterized by poly-arthralgia that can last from weeks to years beyond the acute stage. Patients suffer from joint pains for up to 2 years, depending on their age. Ninety-five percent of infected adults are symptomatic after infection and of these, most become disabled for weeks to months as a result of decreased dexterity, loss of mobility, and delayed reaction. Recurrent joint pain is experienced by 30–40% of those infected. During early epidemics, rare but serious complications of the disease were noted, including myocarditis (inflammation of heart muscle), meningoencephalitis (inflammation of the brain and meninges), and mild haemorrhage. Other complications, such as uveitis and retinitis (inflammation of the eye), have been described.
Death caused by chikungunya infections appears to be rare. However, increases in crude death rates have been reported during the 2004–2008 epidemics. More than half of patients who suffer from severe chikungunya fever are over 65 years old, and more than 33% of them die. Most of these adults have underlying medical conditions and appear to be more likely to suffer complications. Children are also disproportionately affected by severe chikungunya fever.
Pregnancy
During recent outbreaks, it was observed that most chikungunya infections occurring during pregnancy do not appear to result in transmission of the virus to the fetus. However, if the pregnant woman is viremic at the time of delivery, there is a risk for mother-to-child transmission with a vertical-transmission rate of almost fifty percent. Currently, there is no evidence that the virus is transmitted through breast milk.
Often symptoms in infected individuals are mild and most patients recover fully. Infection appears to confer lifelong immunity. Chikungunya virus infections are sometimes confused with dengue viral infection, because both diseases can present with high temperatures and myalgias (muscle pain) in people living in or returning from tropical areas (see table 1). Although these diseases share similar clinical features, prominent and prolonged joint pains are more consistent with chikungunya, whereas haemorrhage is more common in cases of dengue virus infection.
Diagnosis of Chikungunya
Chikungunya infections can be confirmed by the detection of the virus, viral RNA, or specific antibodies in patient samples. The type of testing performed is typically dictated by the timing and volume of samples available. Blood test is the only reliable way to identify chikungunya since the symptoms are similar to much more deadly dengue fever. Common laboratory tests for chikungunya include for instance RT-PCR and serological tests.
RT-PCR
Viral RNA can be easily detected by reverse transcriptase-polymerase chain reaction (RT-PCR) in serum specimens obtained from patients during the acute phase of infection. Chikungunya infections cause high levels of viremia (up to 1x10E6.8 plaque-forming units per mL), which typically last for 4–6 days after the onset of illness. RT-PCR can therefore easily been done within the first 7 days on an acute-phase specimen to confirm chikungunya virus infection. RT–PCR products from clinical samples may also be used for genotyping of the virus, allowing comparisons with virus samples from various geographical sources. PCR results can be available within one to two days.
ELISA
Enzyme-linked immunosorbent assays (ELISA) detect both anti-CHIKV immunoglobulin (Ig) M and IgG antibodies from either acute- or convalescent-phase samples. Serological diagnosis requires a larger amount of blood than the other methods. ELISA results require 2–3 days and the test is quite specific with very little cross reactivity with related alphaviruses. Testing of samples from imported cases found that chikungunya-specific IgM antibodies develop rapidly within a few days after illness onset and persist for several months.
Immunofluorescence assays
Immunofluorescence assays are sensitive and specific but lack the ability to quantify antibodies, are subjective, and require special equipment and training. However, these tests are commercially available and are an option for laboratories that routinely use this method for detection of other infectious agents.
PRNT
Plaque reduction neutralization tests (PRNT) are very useful because they are quite specific for alphaviruses and are the gold standard for confirmation of serologic test results. The major drawback to PRNT is that it requires the use of live virus. The test must be carried out in Biosafety level 3 laboratories (BSL-3) that requires special laboratory containment equipments.
Haemagglutination-inhibition tests
Another way to diagnose the disease is by distinguishing the chikungunya strain by kinetic Haemagglutination-inhibition tests. Chikungunya is confirmed when symptoms such as fever and joint pain seen along with a fourfold Haemagglutination Inhibition antibody difference in paired serum samples. This turns positive within 5 to 8 days of infection.
Testing of both acute- and convalescent-phase samples, collected at least 3 weeks apart, from a patient presenting with a high fever combined with severe joint pain and recent travel to a chikungunya outbreak area should be sufficient to confirm the infection. However, cryoglobulinemia has recently been reported in several patients. Therefore, if a patient presents with appropriate clinical syndrome and travel to an affected area, this should be considered if serologic test results are negative. Health care providers should contact their state or local health department or the CDC for assistance with diagnostic testing.
Treatment of Chikungunya
There are no specific treatments for chikungunya. There is no vaccine currently available. Chikungunya is treated symptomatically, usually with bed rest, fluids, and medicines to relieve symptoms of fever and aching such as ibuprofen, naproxen, acetaminophen, or paracetamol. Aspirin should be avoided. Infected persons should be protected from further mosquito exposure during the first few days of the illness so they can not contribute to the transmission cycle. Since chikungunya is cured by immune system in almost all cases there is no need to worry.
Chloroquine is gaining ground as a possible treatment for the symptoms associated with chikungunya, and as an anti-inflammatory agent to combat the arthritis associated with chikungunya virus. A University of Malaya study found that for arthritis-like symptoms that are not relieved by aspirin and non-steroidal anti-inflammatory drugs (NSAID), chloroquine phosphate (250 mg/day) has given promising results. There is a debate about the appropriateness of chloroquine as treatment for chikungunya. Unpublished studies in cell culture and monkeys show no effect of chloroquine treatment on reduction of chikungunya disease.
According to homeopathic experts effective drugs are available to prevent as well as to speed up recovery from chikungunya. In some of the south Indian cities this type of treatment is tried out. It is claimed that the medicine Eupatorium perf can prevent chikungunya infection. Other medicines prescribed for the disease include Pyroginum, Rhus-tox, Cedron, Influenzinum.
Prevention
Currently there is no prevention for this virus causing disease. There are no anti-viral medications available although your own immune system is the best fighter for this virus. Mosquito repellents can be used to avoid from getting bitten and wearing clothing that is covering your extremities is a big help. Eliminating mosquito-breeding sites is another key prevention measure. The mosquito bites in the day time and reduces its humming of the wings while it is approaching the target and it will often bite from beneath the arms. There are several ways of prevention:
Prevention by Mosquito Control
The best way to reduce mosquitoes is to eliminate the places where the mosquito lays her eggs, like artificial containers that hold water in and around the home. In urban areas, Aedes mosquitos breed on water collections in artificial containers such as plastic cups, used tires, broken bottles, flower pots, etc (see also transmission of chikungunya). Periodic draining or removal of artificial containers is the most effective way of reducing the breeding grounds for mosquitos. Larvicide treatment is another effective way to control the vector larvae but the larvicide chosen should be long-lasting and preferably. There are some very effective insect growth regulators (IGRs) available which are both safe and long-lasting (e.g. pyriproxyfen). For reducing the adult mosquito load, fogging with insecticide is somewhat effective.
To eliminate standing water:
- Unclog roof gutters;
- Empty children's wading pools at least once a week;
- Change water in birdbaths at least weekly;
- Get rid of old tires in your yard, as they collect standing water;
- Empty unused containers, such as flower pots, regularly or store them upside down;
- Drain any collected water from afire pit regularly.
- Natural control - Mesocyclops
In 1998, scientists from the Queensland Institute of Medical Research (QIMR) in Australia and Vietnam's Ministry of Health introduced a scheme that encouraged children to place a water bug, the crustacean Mesocyclops, in water tanks and discarded containers where the Aedes aegyptimosquito was known to thrive. This method is viewed as being more cost-effective and more environmentally friendly than pesticides, though not as effective, and requires the continuing participation of the community.
Even though this method of mosquito control was successful in rural provinces, not much is known about how effective it could be if applied to cities and urban areas. The Mesocyclops can survive and breed in large water containers, but would not be able to do so in small containers of which most urban area have within their homes. Also, Mesocyclops are hosts for the guinea worm, a pathogen that causes a parasite infection, and so this method of mosquito control cannot be used in countries that are still susceptible to the guinea worm. The biggest dilemma with Mesocyclops is that its success depends on the participation of the community. This idea of a possible parasite bearing creature in household water containers dissuades people from continuing the process of inoculation, and without the support and work of everyone living in the city, this method would not be successful.
Prevention by Reducing Mosquito Bites
Prevention of mosquito bites is another way of preventing Chikungunya disease. The adult mosquitoes like to bite inside as well as around homes, during the day and at night when the lights are on. To protect yourself, use insect repellent on your skin while indoors or out, mosquito traps or mosquito nets. When used properly, repellents are safe for kids and adults alike. Keep in mind that even though some of them are classified as pesticides by the Environmental Protection Agency (EPA), repellents don't kill mosquitoes. So you may still see these annoying insects buzzing about. Repellents simply make it more difficult for mosquitoes to find you.
Common insect repellents include:
DEET (N,N-diethylmetatoluamide) blocks a mosquito's ability to find people who've applied it. Apply repellent with a 10% to 30% concentration of DEET to your skin and clothing. Choose the concentration based on the hours of protection you need — the higher the concentration of DEET, the longer you are protected. A 10% concentration protects you for about two hours. Keep in mind that chemical repellents can be toxic, and use only the amount needed for the time you'll be outdoors. Don't use DEET on the hands of young children or on infants younger than age 2 months.
Picaridin. This repellant, also called KBR 3023, offers protection that's comparable to DEET at similar concentrations. It also blocks a mosquito's ability to find people who've applied it. Picaridin is nearly odorless, which may make it a good alternative if you're sensitive to the smells of insect repellents.
Oil of lemon eucalyptus. This plant-based chemical may offer protection that's comparable to low concentrations of DEET. Don't use this product on children younger than 3 years.
Others. Shorter acting repellents that may offer limited protection generally contain plant-based oils such as oil of geranium, cedar, lemon grass, soy or citronella.
When possible, wear also long sleeves and pants for additional protection. Also, make sure window and door screens are secure and without holes. If available, use air-conditioning (see also prevention for travelers.
Clothing tips to keep in mind include:
- Wear long-sleeved shirts;
- Wear socks;
- Wear long pants and consider tucking your pants into your socks;
- Wear light-colored clothing, since mosquitoes are more attracted to darker colors;
- Apply mosquito repellent to your clothing, shoes, and camping gear and bed netting;
- Wear a full-brimmed hat to protect your head and neck;
- Consider wearing a mosquito net to cover your head and face or torso
Disclaimer and Privacy Policy
PLEASE NOTE: Information listed here is not intended to be used as medical advice and should not be classified as such. To safeguard yourself please consult your doctor if you suspect you may have contracted the virus. The information provided by this website is for educational, communication and information purposes only, and does not involve any commercial activity. The information contained in this web site has been adopted from sources other than this site. We have used reasonable efforts to include accurate and up-to-date information without warranties of any kind.
This site cannot and does not warrant the accuracy, completeness, timeliness, non-infringement, merchantability or fitness for a particular purpose of any information available through this site or any links and disclaims any opinions expressed that are not in-keeping with standard medical practice. Safeguard yourself and consult your doctor if you suspect you may have contracted the virus.
*Some information sourced from http://www.chikungunyavirusnet.com
http://www.chikungunyavirusnet.com
*Safeguard yourself and consult your doctor if you suspect you may have contracted the virus.